Since general practitioners are now treating a lot of the easier aligner cases themselves, orthodontists are now primarily treating more complex cases, thereby totally redefining the “bread and butter” of what orthodontists typically treat. These are cases that orthodontists previously referred for surgery and/or cases that could only be treated with braces, taking 3 to 4 years to complete. Many patients prefer the aesthetic appeal of clear aligners instead of traditional braces and are unwilling to remain in treatment for multiple years, no matter how complex the case. These same patients want to improve their smiles for health, social, or professional reasons and they shouldn’t have to compromise on their treatment goals and expectations. That’s why it’s important now more than ever for orthodontists to develop innovative techniques and to consider how technologies can help them achieve a quality clinical result in a timely manner while reducing discomfort for patients. This case shows several of the technologies and products that we use in our practice that help us deliver the quality clinical results our patients expect.
Clinical Findings

We diagnosed her as Class I posterior occlusion with severe lower crowding, vertical maxillary excess, and lip incompetence at rest. She had 5 mm of anterior overjet, moderately deep anterior overbite, mild upper crowding, and thin biotype. Radiographic findings were positive for flattened condylar heads. Three of the third molars were impacted: #1, #17, and #32. Since the third molars were asymptomatic, we opted to leave them in situ.
Treatment Plan
Our treatment plan for her included clear aligners (Invisalign®, Align Technology), temporary anchorage devices (TADs), and vibratory acceleration (AcceleDent®, OrthoAccel Technologies) to align the teeth, improve the smile width, and decrease the amount of gingival display. There were 28 upper and lower aligners in the first round, including three for overcorrection that were not used. We did 0.5 mm of interproximal reduction (IPR) between the lower anterior teeth. We initially placed her on a 7-day aligner change schedule and the patient used AcceleDent for 20 minutes daily.
While it’s at the doctor’s discretion, Invisalign’s weekly aligner change recommendation is primarily appropriate for patients with excellent oral hygiene and compliance as well as Class I patients with mild crowding and whose treatment does not require addressing difficult tooth movements with aligners such as rotations, extrusions, and significant root movements.1 Since this particular case did not meet these parameters, and to avoid 2-week aligner changes, the patient was prescribed AcceleDent and instructed to change aligners weekly. We recommended that the patient use AcceleDent for clinical efficiency and to reduce any discomfort she may have experienced because of tooth sensitivity related to a chronic sinus problem.
To the best of our knowledge, this was the first case that performed full maxillary impaction non-surgically with only TADs and aligners. Our treatment plan design was a modification of a technique first shown in a lecture by John Pobanz, DDS, MS, who used a combination of TADs and braces for maxillary impaction. In addition to aligners and TADs, we incorporated AcceleDent.2
At the first appointment, the patient received the first three sets of aligners with instructions. During the patient’s second appointment, we did IPR and placed elastic hooks, attachments, and five TADs to assist with anterior and posterior maxillary impaction. We’ve since updated our protocol and TADs are now placed by an oral surgeon between the first and second appointment. Whenever possible, we now delay IPR until refinement aligners.
Using a manual driver (SuperTAD Rotatable Handle with SuperTAD Driver Straight Shaft, Ortho SuperTAD), we placed two 2 x 12 mm stainless steel TADs (“SuperTAD 1”, Ortho SuperTAD) into the infrazygomatic crest at the mesiobuccal cusp of the first molars with 2 to 3 mm of screw remaining exposed. Additionally, two temporary anchors in titanium dimensions 1.5 x 6 mm were placed between the roots of the upper laterals and upper canines as apically as possible (Tomas-Pin SD 06, Dentaurum USA) using the Orthonia Electronic Torque Driver (RMO®) set to 15 NcM with the Tomas-Driver (302-004-50, Dentaurum USA). For patient comfort, we later moved the right anterior anchor down occlusally away from the vestibule and added flowable composite (Transbond LT, 3M Oral Care) over the head of the screw to the two anterior TADs for lip comfort. A 1.5 x 8 mm stainless steel palatal TAD (“SuperTAD 3”, Ortho SuperTAD) was placed at the midline raphe at the level of the second premolars. For the palatal TAD, a 19 x 25 stainless steel wire was custom bent into a “dumbbell attachment,” which is a technique adopted from Pobanz. The wire was then inserted into the slot of the palatal TAD and glued into place with Heliosit adhesive (Ivoclar Vivadent). A combination of freehand composite buttons and Caplin hooks (Dentsply Sirona) were used to connect the TADs to the teeth directly using c-chains (Ormco Corp). In month 6, we replaced the c-chains with stainless steel ties to maintain the intrusion while fine tuning the impaction for the last 5 months of treatment.
For the refinement phase, there were 29 upper and 26 lower refinement aligners, including three for overcorrection of space closure that were not needed. We had the patient switch to 4-day aligner changes at refinement aligner #7 due to good compliance with both aligner wear and AcceleDent use.
Gingivectomy with a soft tissue diode laser (ProSoft NV) was performed at the end of treatment to help expedite soft tissue remodeling after intrusion was complete. This was 1.2 watts of continuous laser and we used Profound—PET gel topical anesthetic, which is a combination of lidocaine (10%), prilocaine (10%) and tetracaine (4%) from a local compounding pharmacy. The laser allowed us to uncover the teeth quickly without waiting on the gums to remodel spontaneously.
For retention, a lower lingual retainer (Wildcat stainless steel .0215 twistflex, Dentsply Sirona) was bonded to all anterior teeth canine-to-canine using flowable composite (Transbond LT, 3M Oral Care). For the upper arch, the patient was instructed to use an upper Invisalign retainer for sleeping. Additionally, the patient was given bleach at the end of treatment to whiten her teeth. The result appears stable thus far, as we have seen no clinical change visually in the 2 years post treatment.
Results
We originally estimated that this treatment would take 18 to 24 months; with our approach, integrating AcceleDent and TADs with Invisalign, treatment was complete in 10 months. We use OrthoFi for patient financing, which is equipped to manage payment plans that extend beyond treatment time. This payment flexibility together with clinical acceleration assists us in meeting patient demand for excellent results in a more efficient timeframe while maintaining a fee equitable to the results obtained.
Approximately 4 mm of maxillary impaction was achieved with no significant change to the root structure in the x-ray. The impaction of the maxillary teeth created an auto rotation of the mandible which decreased the lower vertical face height, improved the chin prominence, and allowed the lips to comfortably come together when the mouth is closed.
In addition to achieving ideal alignment, the arch width on the upper and lower arches was improved and we resolved the excess overjet. The significant anterior deep bite was corrected and interdigitation of the posterior teeth was maintained, which is challenging in a case involving mandibular autorotation.
Compliance was good throughout treatment and this was assisted by Orthodontext. We have used the Orthodontext system for several years to send patients text reminders to change their aligners (or elastics, oral hygiene, etc). This is particularly helpful for accelerated cases where aligner changes can occur at unusual intervals such as 4- or 5-day changes.
Discussion
The large majority of orthodontists would have recommended orthognathic surgery for maxillary impaction to correct the excess gingival display. The majority of surgeons still require traditional braces with posterior bands in order to ensure stability immediately post-surgery. At the start of this patient’s treatment in 2015, very few orthodontists were attempting non-surgical maxillary impactions and there were no examples in the lectures or literature we had seen using clear aligners for full maxillary impaction of both the anterior and posterior teeth. For this particular patient, her busy travel schedule for work did not allow for taking time off for surgery nor did it lend itself to the potential complications of full fixed appliances in addition to the TAD setup.
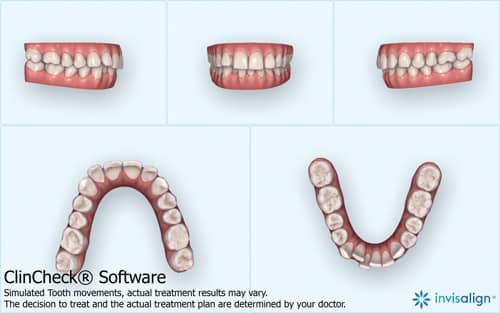
As is true with every case, designing the treatment plan accurately and thoroughly in the ClinCheck is important. Since the goal was full maxillary impaction, it was not necessary to make any significant specific accommodations in the ClinCheck for the impaction protocol, other than requesting cutouts where possible. One of the benefits of prescribing AcceleDent is the increased predictability of the tracking of the tooth movement in the aligners, which is particularly important in a case with complex auxiliaries such as this patient. Over the past few years of using AcceleDent’s SoftPulse Technology for virtually all of our Invisalign patients, we have been able to eliminate nearly all of the “overcorrections” we used to program into the ClinCheck software. In our experience, the patient use of AcceleDent with their aligners helps ensure all of the tooth movements that are planned in the ClinCheck software are fully expressed during treatment. OP
References
1. Align Technology introduces one-week aligner wear for Invisalign® Teen and Full products. 2016. (News Release)
2. Pavlin D, et al. Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: A double-blind, randomized controlled trial. Seminars in Orthodontics. 2015; 21(3): 187-194.
3. Lobre W, et al. Pain control in orthodontics using a micropulse vibration device: A randomized clinical trial. The Angle Orthodontist. 2016; 86(4): 625-630.
4. Pobanz, J. A winning combination. OrthoTown Magazine, September 2016.
5. Pobanz, J. TADs case presentation. OrthoTown Magazine, March 2012.