Obstructive sleep apnea (OSA) is an inherited progressive problem that has become a major healthcare issue in the United States and throughout many other developed nations. It is one category within a more global spectrum of conditions known as sleep disordered breathing (SDB). OSA is thought to begin as “simple snoring” and progress until developing into full-blown obstructive sleep apnea. It is traditionally treated with continuous positive air pressure (CPAP) or some form of mandibular repositioning device. Various surgical procedures have also been utilized to address the underlying anatomic issue(s).
These various approaches are effective because OSA is a condition resulting from a combination of anatomic features that create an obstruction or reduction in airflow at some level in the maxillofacial complex. For many patients, orthodontists have a unique opportunity to provide definitive correction of the underlying problems because we are the only specialty that routinely changes the morphology of the maxillofacial complex without surgery. In many ways, OSA is a medical condition with an orthodontic solution. It is important to note that in every situation, only a physician can make the diagnosis of snoring or obstructive sleep apnea even though we as dentists provide much of the treatment. The reason this is important to both us and the patient is that even though OSA is the most common form of sleep disordered breathing, it is critical to rule out such entities as central apnea.
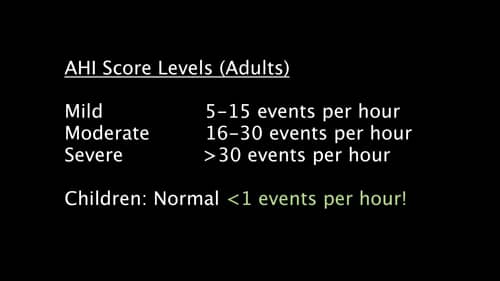
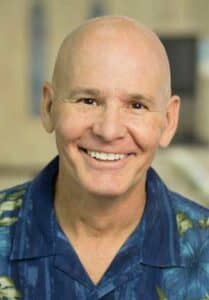
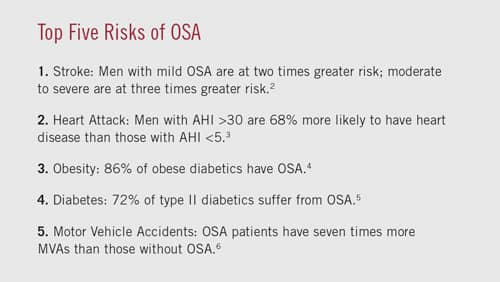
Figure 1: The apnea-hypopnea index (AHI) is used to measure the number of times breathing pauses or severely slows per hour of sleep.
OSA is categorized in adults as normal, mild, moderate, or severe depending on how many obstructive events occur per hour while sleeping. These events are described as apneas or hypopneas. An apneic event is the cessation of breathing for greater than 10 seconds. A hypopnea is the reduction of blood oxygen (pO2) resulting in a 4% or greater desaturation. Although apneas were previously considered more damaging than hypopneas, current thinking and evidence is that over time hypopneas are just as damaging as apneas. The apnea hypopnea index (AHI) is used to define the severity of the problem. AHI is calculated by counting the number of such events all night while sleeping and dividing by the number of hours the patient slept producing an average count per hour. For adults, the categories are as follows: 0>5 normal, 5>15 mild, 15>30 moderate, and >30 severe. In children, the AHI should always be less than 1 (Figure 1 and Figure 2).
Another classification is the respiratory disturbance index (RDI). RDI is a measure that uses the AHI and adds the number of respiratory effort related arousals (RERAs) to the calculation. A RERA occurs when the patient strains to inspire air, but, due to the blockage, is unable to breathe without an abnormally excessive effort. This eventually results in a partial awakening caused by a jolt of adrenaline that results in increasing muscle tone in the airway to allow air to enter. Imagine how you feel a few seconds after being startled to the point of a major adrenaline release. Now imagine that happening 30 or more times per hour! These RERAs result in patients waking up exhausted due to the repeated systemic catecholamine attack combined with the lack of time spent in deep sleep.
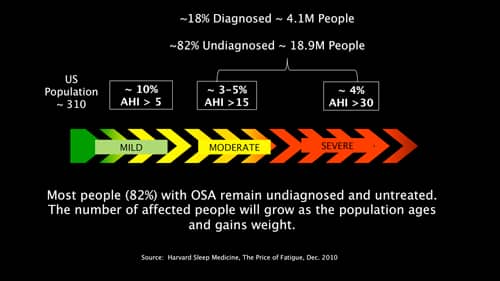
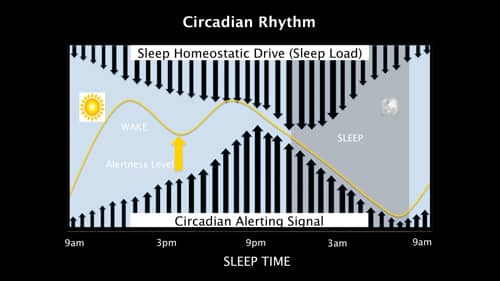
Deep sleep is one portion of the sleep architecture described as the ultradian rhythm. Unlike the well-known 24-hour circadian rhythm, which is the wake-sleep cycle, the ultradian rhythm is the 90 to 110 minute cycle of light sleep through REM sleep that normally happens each night. It is the ultradian rhythm that is significantly disrupted by sleep disordered breathing (Figures 3 and 4).
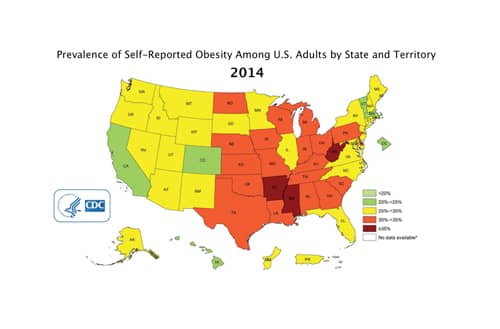
Figure 5: Obesity is the single biggest contributor to OSA, as the excess weight results in fat deposits in tissues throughout the body, including the tongue and the posterior pharyngeal wall.
Causes of Obstructive Sleep Apnea
The single biggest contributor to OSA is obesity. According to the Centers for Disease Control and Prevention, the number of medically obese people in the United States has continuously increased over the course of the past 25 years with the latest data having three states with over 35% of the population medically obese (Figure 5).1 The reason that obesity is such a big contributor—that sometimes is less than obvious—is that as one gains excess weight, fat is deposited in all tissues throughout the body, including the tongue and the posterior pharyngeal wall. As weight increases, the size of the airway decreases. Imagine a doughnut being placed into hot oil; not only does the external diameter of the doughnut increase, the size of the “doughnut hole” decreases as the dough swells. Other anatomical causes of OSA include, but are not limited to, enlarged adenoids, enlarged tonsils, retrognathic mandible, midface deficiency, deviated septum, or any combination of the above that forces the tongue into a posterior or inferior position that may reduce the size of the airway.
Physiologic Effects of Sleep Disordered Breathing
Because of the repetitive and chronic nature of OSA, virtually every system in the body is affected. There are two major events that negatively affect the physiology of patients who suffer from OSA, hypoxia and repeated adrenaline release (RERAs). The physiologic effects are cumulative and can be devastating. The reader can see in Table 1 that OSA is a leading contributing factor for stroke, increased blood pressure, heart attacks, diabetes, and motor vehicle accidents. The Wisconsin Cohort Study showed that individuals with an AHI of greater than 30 had a less than 60% chance of living more than 15 years. As was mentioned previously, the single biggest contributor to OSA is obesity. Unfortunately, when one suffers from untreated OSA, it is virtually impossible to lose weight so it becomes a vicious cycle. The body of someone suffering from OSA is less responsive to levels of leptin, the hormone that triggers the sensation of satiation; at the same time, the body produces increased levels of ghrelin, which tells us we are hungry. The combination of these two alterations to normal hormonal balance causes the body to store everything that is eaten as adipose tissue. Until normal sleep patterns are returned, it becomes almost impossible to lose weight, and unless weight is lost, the cycle will continue. That is why some form of intervention is required to establish healthy sleep that then allows the patient to lose weight.
In children with sleep disordered breathing, cognitive development is negatively affected. Gozal and Pope described a learning deficit wherein the child’s cognitive development is delayed; and although the developmental curve returns to the normal slope once treated, the differential is never recovered. According to Ronald Chervin, MD, MS, a 2012 study shows clearly that SDB symptoms precede behavioral problems by up to several years and strongly suggests that SDB symptoms are causing those problems. In fact, it has been demonstrated that the IQ of children with SDB may be as much as 16 points lower than that of their normal peers, which ironically is the same differential that is used to qualify children for special education services. Many times children are misdiagnosed as ADHD when in fact they have some form of SDB.
Recognition and Diagnostic Aids
In 2012, the American Academy of Pediatrics issued the following statement: “All children should be screened for breathing problems and if signs and symptoms are present, they should be tested for sleep disordered breathing (SDB) and sleep apnea.” Unfortunately, my experience has been that most pediatricians do not follow these guidelines. As orthodontists, it is really quite simple to add screening for SDB into our already thorough exam of the maxillofacial structures. It starts with some simple questions on sleepiness and behavior (Pediatric Sleep Questionnaire for children and the Epworth Scale for adults, both of which are readily available on the web). Another tool we have at our disposal that is extremely effective in screening for airway issues is to measure the minimum cross-sectional area (MCA) of the pharyngeal airway on a CBCT using software such as InVivo Anatomage (Anatomage Inc) or Dolphin 3D (Dolphin Imaging and Management Solutions). Although no specific correlation has been established, the MCA information is an excellent screening tool in that we know a small airway in an awake upright position will only be more constricted when asleep in a supine position. The minimum dimension we look for is 10 times the patient’s age up to age 20. If the clinical examination of the patient reveals something like large tonsils, or there are other indications from the interview, CBCT image assessments, or exam, then a home sleep test (HST) such as the NOX-T3 portable sleep monitor (Becton, Dickinson and Co) may be indicated. Although a dentist can issue the HST in most states, a qualified physician MUST interpret the results. You can use either a local board-certified sleep physician or an online diagnostic service to obtain the interpretation and perhaps a prescription for treatment along with the diagnosis. Once the diagnosis is obtained, there are several avenues for treatment.
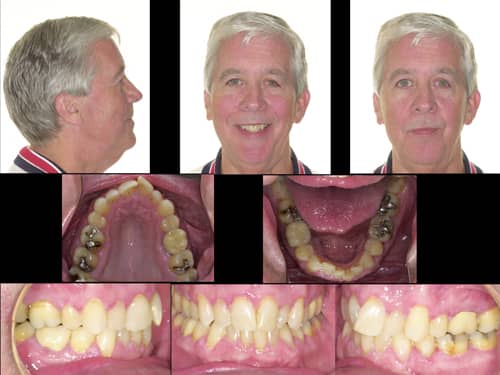
Figure 6: Jerry, a patient, was CPAP dependent and had an AHI=52 when he sought orthodontic treatment.

Figure 7: Jerry was treated with a nighttime sleep appliance that also serves as his retainer. Post-treatment AHI=5.8.
Treatment of Obstructive Sleep Apnea
Currently, the gold standard for OSA treatment is CPAP. Unfortunately, it has been reported that up to 70% of patients issued a CPAP device fail to use it on a regular or routine basis. Once CPAP has failed, most medical insurance companies will pay for an oral appliance. All oral appliances have similar characteristics and must be approved by the FDA. They all hold the mandible down and forward (think of the mandibular position used for CPR to open the airway) and must be titratable. The shortcoming with many mandibular repositioning appliances is that they may lead to sore TM joints, masticatory musculature, or tooth movement.
In addition to CPAP or appliance treatment, various surgical approaches have been used to treat OSA. One such approach is the uvulopalatopharyngoplasty (UPPP). This procedure has a difficult recovery period and only a 50% success after 5 years. A more extensive surgical procedure that is almost always successful is the maxillomandibular advancement surgery (MMA). This procedure is similar to traditional orthognathic two jaw surgery, but it is done with a counterclockwise rotation of the occlusal plane in order to maximize the increase in the minimal cross-sectional dimension of the airway. Most times this is done in conjunction with an orthodontist. The current recommendation is to perform this procedure using a technique called surgery first, where the braces are placed the day prior to surgery and then the teeth are positioned orthodontically beginning 1 month post-surgery. Another surgical procedure that is commonly used is the tonsillar-adenoidectomy (T&A). A recent study at Stanford University demonstrated that most patients saw improved airways with T&A alone; however, maxillary expansion, when performed with or without a T&A, was the most successful treatment.
The reason maxillary expansion is so successful is that it creates more room for the tongue. In much the same way mandibular repositioning appliances make more room for the tongue in two planes of space, an orthodontist using maxillary expansion along with some form of bite opening and mandibular repositioning creates more room for the tongue in all three planes of space. This can be done in any number of ways, including: RPE, Herbst, Twin-Block, nitanium expander, Carriere® Motion™ II (Henry Schein Orthodontics), fixed appliances, etc. The point is that many orthodontists have been providing treatment that has improved airways without even knowing it.
Jerry is just such a patient. He was treated 10 years ago and was weaned off his CPAP to a nighttime sleep appliance that also serves as his retainer. This was done before the author had much awareness of OSA and certainly did not plan orthodontic treatment around it (Figures 6 and 7).
Summary
Obstructive sleep apnea is a major global health issue. Orthodontists are in a unique position to recognize, screen, and treat patients with sleep disordered breathing, including OSA. Working with our medical physician partners, who will diagnose OSA and other conditions, we can become an ally in improving the health and well-being of these patients. I feel that by being educated in sleep disordered breathing, orthodontists have the ability to benefit patients’ health and improve their lives in ways we never have before. We face ever-increasing competition from primary care dentists, along with an increasing number of new graduates. Given this, gaining expertise in treating patients, young and old, with OSA serves to open new and broader paths for us and expands our role in the healthcare arena. OP
References
- Prevalence of Self-Reported Obesity Among U.S. Adults by State and Territory, BRFSS, 2014, Behavorial Risk Factor Surveillance System, CDC.
- OSA and increased risk of stroke. (April 2010) Sleep Apnea Tied to Increased Risk of Stroke, National Institutes of Health.
- OSA and increased risk of heart failure. Shahrokh – Javaheri, M.D. (2013). Basics of Sleep Apnea and Heart Failure, CardioSource.
- OSA tie to obesity. Fritscher LG1, Mottin CC, Canani S, Chatkin JM, Jan. 2007. Obes Surg. 17(1):95-9. Obesity and obstructive sleep apnea-hypopnea syndrome: the impact of bariatric surgery.
- OSA tie to diabetes. Brooks B, Cistulli PA, Borkman M, Ross G, McGhee S, Grunstein RR, Sullivan CE, Yue DK (Dec. 1994) Obstructive sleep apnea in obese noninsulin-dependent diabetic patients: effect of continuous positive airway pressure treatment on insulin responsiveness. J Clin Endocrinol Metab. 79(6):1681-5.
- OSA tie to increased motor vehicle accidents. (Aug. 1988) Am Rev Respir Dis., 138(2):337-40.