The development of a Class III malocclusion is often hereditary and varies greatly within different races and geographic regions. Southeast Asian populations have the highest prevalence of Class III malocclusion (13% to 27%), while Indian and Caucasian populations have a lowest prevalence (1% to 5%). Its occurrence is often due to a combination of dental and skeletal components. The most common skeletal relationship is a combination of maxillary retrusion (hypoplasia) and mandibular protrusion (prognathia) being present in approximately one-third to one-half of all adult Class III patients.

Neal D. Kravitz, DMD, MS, is a Diplomate of the American Board of Orthodontics, as well as a clinical faculty member at Washington Hospital Center. Kravitz has been published in numerous orthodontic journals, books, and educational materials. He lectures throughout the country and internationally on modern advancements in orthodontics, lingual orthodontics, treatment planning, and practice management. He currently maintains two orthodontic practices in South Riding, Va, and White Plains, Md.
In patients with mild maxillary deficiency, early treatment during the elementary school years with protraction face mask therapy can eliminate an anterior crossbite, improve facial esthetics, and minimize dental compensation, though it is debatable what long-term effect this provides to the growth potential of the nasomaxillary complex. However, a Class III malocclusion due to significant mandibular prognathism is more effectively treated after the completion of skeletal growth with orthognathic surgery. Simply put, modest growth modification can be performed in the maxilla, but there is little if anything we can do to restrict the development of the mandible. For late adolescent or adult patients with a moderate Class III malocclusion who refuse orthognathic surgery, orthodontic treatment with mandibular bicuspid extraction may be a viable alternative. Extraction of the mandibular bicuspids, while maintaining a full complement of maxillary teeth, compensates for the skeletal imbalance by retracting the lower incisors to achieve positive overjet. Despite the proficiency of this technique, it is not without its challenges. This case report will review Class III camouflaging with mandibular bicuspid extraction, as well as examine proper patient selection and treatment biomechanics.
Diagnosis and Etiology
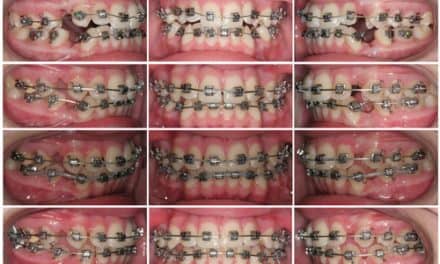
A 14.1-year-old adolescent female presented to our office for a Phase 2 orthodontic consultation, following early treatment at a different office. She presented with a slightly concave soft-tissue profile including flat malar eminences with good facial symmetry, with the maxillary dental midline left of the facial midline. Intraoral examination revealed full eruption of the permanent dentition including the second molars, edge to edge occlusion with the maxillary lateral incisors and the mandibular left central incisor in anterior crossbite, distal-out malrotation of both mandibular canines, and maxillary dental midline left of the mandibular dental midline (Figure 1).
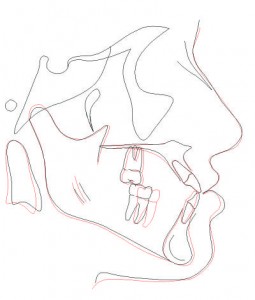
Cephalometric analysis confirmed a mild Class III skeletal relationship (SNA: 79o; SNB: 80o) due to maxillary hypoplasia (Figure 2). Panoramic evaluation revealed presence of all third molars, good bone and root health, and acceptable condylar head shape bilaterally (Figure 3). Study model analysis revealed a full-step Class III malocclusion bilaterally, tapered-maxillary arch, negative overjet (-1 mm), inadequate overbite, and moderate crowding.
Treatment Objectives
The parents and I identified four primary treatment objectives:
- Establish functional canine Class I occlusion with positive overjet;
- Resolve maxillary and mandibular crowding;
- Coincide dental midlines and align dental midlines with the facial midline; and
- Maintain or improve soft-tissue facial esthetics.
Treatment Alternatives
The patient presented to our office already informed of the benefit of orthognathic surgery by her previous orthodontist. However, the family requested only nonsurgical treatment alternatives. Therefore, our treatment options were limited to (1) lower reproximation with Class III directional elastics, (2) mandibular incisor extraction, (3) maxillary second bicuspid and mandibular first bicuspid extraction, or (4) camouflaging with mandibular bicuspid extraction only. With regard to the first three treatment options, I was concerned that I might fail to achieve positive overjet due to the severity of the Class III molar relationship, the extent of mandibular anterior crowding, and the anticipation of further mandibular growth. Therefore, a treatment plan that included mandibular first bicuspid extraction only was agreed upon.
Figure 4: Unilateral Class II biomechanics with a maxillary 0.018″ stainless steel archwire and a mandibular 0.017″ x 0.025″ stainless steel archwire to coincide dental midlines. The mandibular second molars were bonded shortly after this visit.
Treatment Progress
The patient was bonded with fixed, 0.018? slot preadjusted edgewise appliances (Rocky Mountain Orthodontics) excluding the mandibular first premolars. On the bonding appointment, a referral was written to the oral surgeon for extraction of the mandibular first premolars and the maxillary third molars. The mandibular third molars were to be preserved, allowing for their eruption into occlusion following anchorage loss of the mandibular first and the second molars.
The parents opted to delay extraction of the maxillary third molars until the end of treatment. Following extraction of the mandibular first premolars, archwires were progressed to stainless steel to begin space consolidation with elastic chain. After 9 months of orthodontic treatment, positive overjet was achieved. Once enough overjet was established, the patient transitioned to Class II biomechanics with a maxillary 0.018?. stainless steel archwire, a mandibular 0.017? x 0.025? stainless steel archwire, and Class II directional interach elastics (3/16?, 5 oz) (Figure 4). Maxillary anterior reproximation further uprighted the maxillary incisors in the dentoalveolus. After acceptable incisor angulation was achieved, triangle elastics (3/16?, 5 oz) and minimal occlusal equilibration helped settle the posterior occlusion. At the debonding appointment, panoramic evidence confirmed horizontal impaction of the mandibular left third molar, necessitating its extraction along with the maxillary third molars. Retention included upper and lower lingual retainers with overlay polyurethane aligners to be worn at night to prevent supraeruption of the maxillary second molars. The total length of Phase 2 treatment was 18 months.
Treatment Results
The results of our treatment were an acceptable Class I canine occlusion with maintained facial balance (Figure 5). Positive overjet was achieved by retracting the mandibular anterior teeth into the extraction space, and Class II treatment biomechanics minimized excessive retroclination of the mandibular incisors. Evaluation of pretreatment and posterior treatment cephalometric measurements showed mandibular anterior retraction, mandibular molar anchorage loss, and minimal changes to lip positive relative to the Esthetic Line despite further mandibular growth (Figure 6).
Discussion
A severe Class III malocclusion due to mandibular prognathia is best treated after the completion of skeletal growth with orthognathic surgery. However, this treatment can be challenging for patients and families to accept. Complications of orthognathic surgery include morbidity from general anesthesia, inferior alveolar nerve paresthesia, unfavorable mandibular fracture, facial asymmetry, surgical relapse, damage to teeth, delay in treatment until skeletal maturation, time away from school or work, and challenges with insurance reimbursement.
Though extraction of mandibular bicuspids provides a viable alternative to orthognathic surgery, successful dental camouflaging is dependent on proper patient selection. Simply, some cases of prognathia are too severe to be treated without surgery. Patients who are acceptable candidates for nonsurgical dental camouflaging may present with some of the following characteristics: (1) no more than a full-step Class III molar malocclusion (ie, mesial buccal cusp of the maxillary first molar in the distal groove of the mandibular first molar), (2) less than 5 mm of negative overjet, (3) less than 3 mm of anterior open bite, (4) mandibular dental protrusion, (5) mandibular anterior crowding, (6) acceptable facial esthetics, and (7) thick tissue biotype with good periodontal health and dentoalveolar thickness.
The decision of whether to extract the mandibular first or second bicuspids is dependent on the extent of mandibular anterior crowding and the severity of negative overjet. I favor extraction of the mandibular second bicuspids when mandibular anterior crowding is minimal and negative overjet is less severe—for example, during retreatment cases following late mandibular growth. Mandibular second bicuspid extraction is also more acceptable to patients esthetically, as extraction spacing is further toward the back of the mouth. However, the primary advantage of second bicuspid extraction is that it minimizes excessive retroclination of the mandibular incisors. In our case report, first bicuspids were extracted due to the presence of mandibular anterior crowding and the anticipation of further mandibular growth.
Figure 7 (top): Class II Camouflage; (middle): Class III Camouflage; (bottom): Class III Camouflage Supraeruption
To avoid excessive retroclination of the mandibular incisors, I combine mandibular dental camouflaging with Class II treatment biomechanics. In our case report, once sufficient positive overjet was achieved, a maxillary round stainless steel archwire and a mandibular heavy rectangular stainless steel archwire were placed with Class II directional elastics to retrocline the maxillary incisors, procline the mandibular incisors, and protract the mandibular molars. Maxillary anterior reproximation further improved angulation of the maxillary incisors despite the presence of pretreatment crowding.
In addition to implementing Class II treatment biomechanics, I also bond maxillary and mandibular second molars. More than 80% of orthodontists fail to bond second molars during orthodontic treatment. However, this step is imperative during dental camouflaging. Anchorage loss from anterior retraction results in separation of the first and second molars. Incorporating mandibular second molars into the archwire avoids unwanted posterior spacing, though it increases anchorage.
To prevent excessive anterior retraction, I first consolidate extraction spaces with an elastic chain first molar to first molar, and only begin protracting the second molars once I have started interarch elastics. Furthermore, if the mandibular third molars have not yet erupted into occlusion, the maxillary second molars are left hanging without an occlusal stop. Bonding the maxillary second molars from the start of treatment avoids unwanted supraeruption, which may cause bite opening after the mandibular third molars erupt.
Perhaps the greatest challenge with Class III dental camouflaging is establishing proper maxillary first molar intercuspation. In contrast, Class II dental camouflaging with maxillary bicuspid extraction results in good maxillary first molar intercuspation, with the mesial buccal cusp occupying the embrasure between the mandibular second premolar and first molar (Figure 7 top). Theoretically, in Class III dental camouflaging, the mesial buccal cusp of the maxillary first molar should sit within the distal groove of the mandibular first molar or the embrasure between the first and second molar (Figure 7 middle).

Figure 8: Final study model. Note the occlusal stop for the maxillary second molar provided by the distal cusp of the mandibular second molar.
This enables the distal cusp of the mandibular second molar to provide an occlusal stop for the maxillary second molar (Figure 8). Oftentimes, the mesial buccal of the maxillary first molar cusp sits atop the mesial buccal cusp of the mandibular second molar, creating an end-on molar relationship, which causes the maxillary second molar to hang off the occlusion (Figure 7 bottom). Therefore, it is important to control the vertical position of the maxillary second molars during treatment and retain this position at the end of treatment with a full-coverage polyurethane retainer in the absence of mandibular third molar occlusal contact.
Conclusion
Mandibular premolar extraction using Class II treatment mechanics can provide an acceptable alternative to orthognathic surgery. Though effective in achieving positive overjet, the challenge with this treatment lies in avoiding excessive retroclination on the of mandibular incisors, settling the posterior occlusion, and preventing supraeruption of the hanging maxillary second molars. OP